
ERNESTO® Rotwein-/Weißw.-/Sekt-/Wassergläser
14,99 €
Lidl Online-Shop
ab 5,95 Versandkosten

Ewers Strickstrumpfhose Ewers Mädchen 2er Pack Str...
14,75 €
OTTO
ab 4,20 Versandkosten

Artland Glasbild Wein - Rotwein, Getränke (1 St),...
27,99 €
OTTO
ab 2,95 Versandkosten
Artland Glasbild Wein - Rotwein, Getränke (1 St),...
65,99 €
OTTO
ab 2,95 Versandkosten
Artland Glasbild Wein - Rotwein, Getränke (1 St),...
130,99 €
OTTO
ab 2,95 Versandkosten

Artland Glasbild Wein - Rotwein, Getränke (1 St),...
120,99 €
OTTO
ab 2,95 Versandkosten

Artland Glasbild Gläser Rotwein auf altem Fass, Ge...
37,99 €
OTTO
ab 2,95 Versandkosten

Artland Glasbild Gläser Rotwein auf altem Fass, Ge...
27,99 €
OTTO
ab 2,95 Versandkosten
Artland Glasbild Gläser Rotwein auf altem Fass, Ge...
120,99 €
OTTO
ab 2,95 Versandkosten
Artland Wandbild Gläser Rotwein auf altem Fass, Ge...
19,99 €
OTTO
ab 2,95 Versandkosten
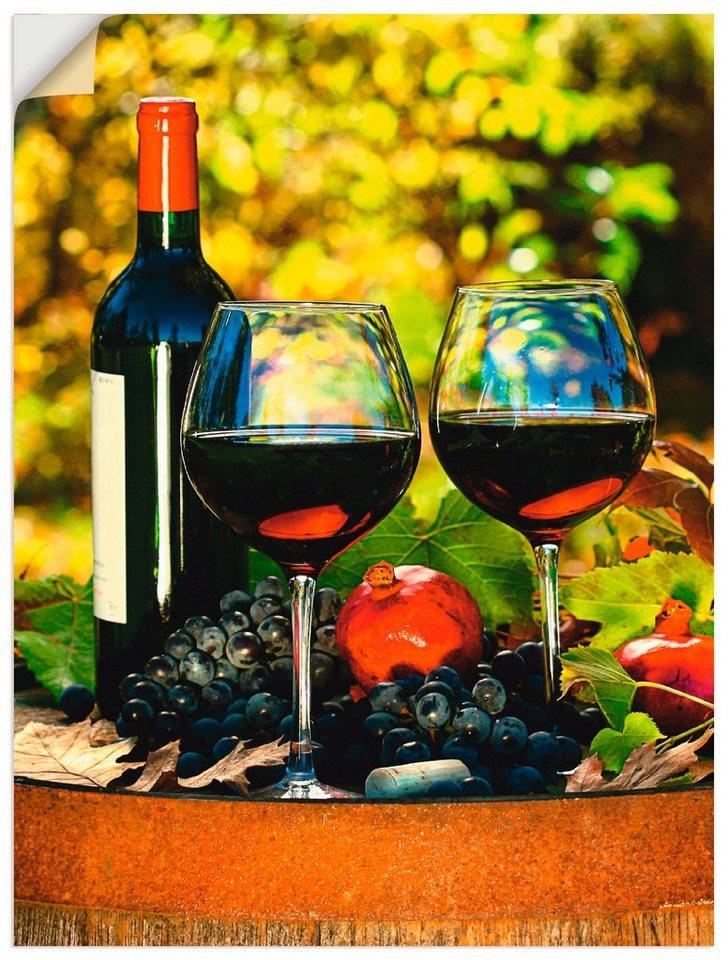
Artland Wandbild Gläser Rotwein auf altem Fass, Ge...
37,99 €
OTTO
ab 2,95 Versandkosten

ERNESTO® Rotwein- / Wassergläser, Kristallglas
11,99 €
Lidl Online-Shop
ab 5,95 Versandkosten
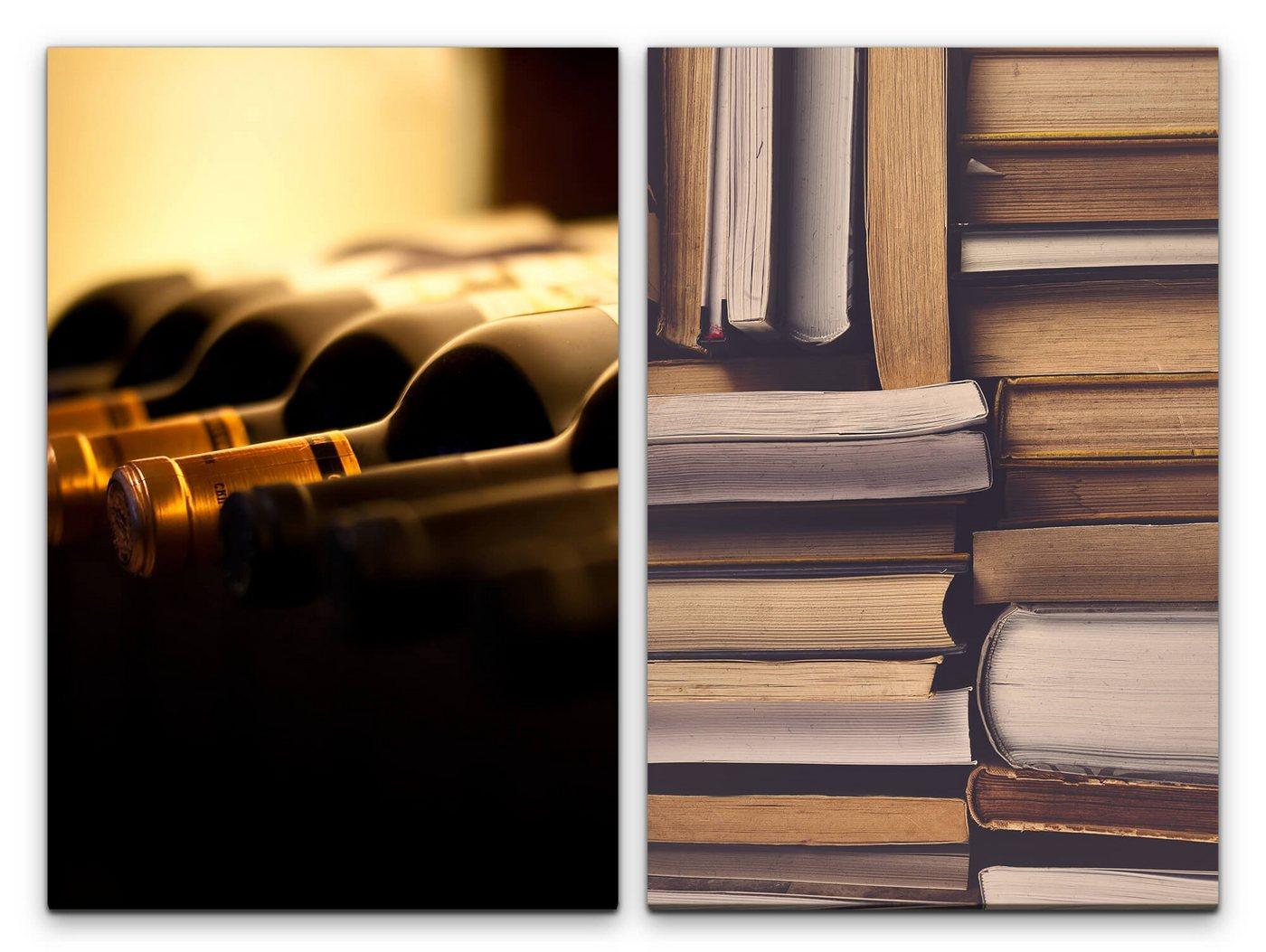
Sinus Art Leinwandbild 2 Bilder je 60x90cm Bibliot...
37,00 €
OTTO
ab 7,00 Versandkosten

Sinus Art Leinwandbild 2 Bilder je 60x90cm Klavier...
37,00 €
OTTO
ab 7,00 Versandkosten
Sinus Art Poster Künstlerische Fotografie Rotwein...
12,00 €
OTTO
ab 7,00 Versandkosten

Artland Holzbild Wein - Rotwein, Getränke (1 St),...
43,99 €
OTTO
ab 2,95 Versandkosten
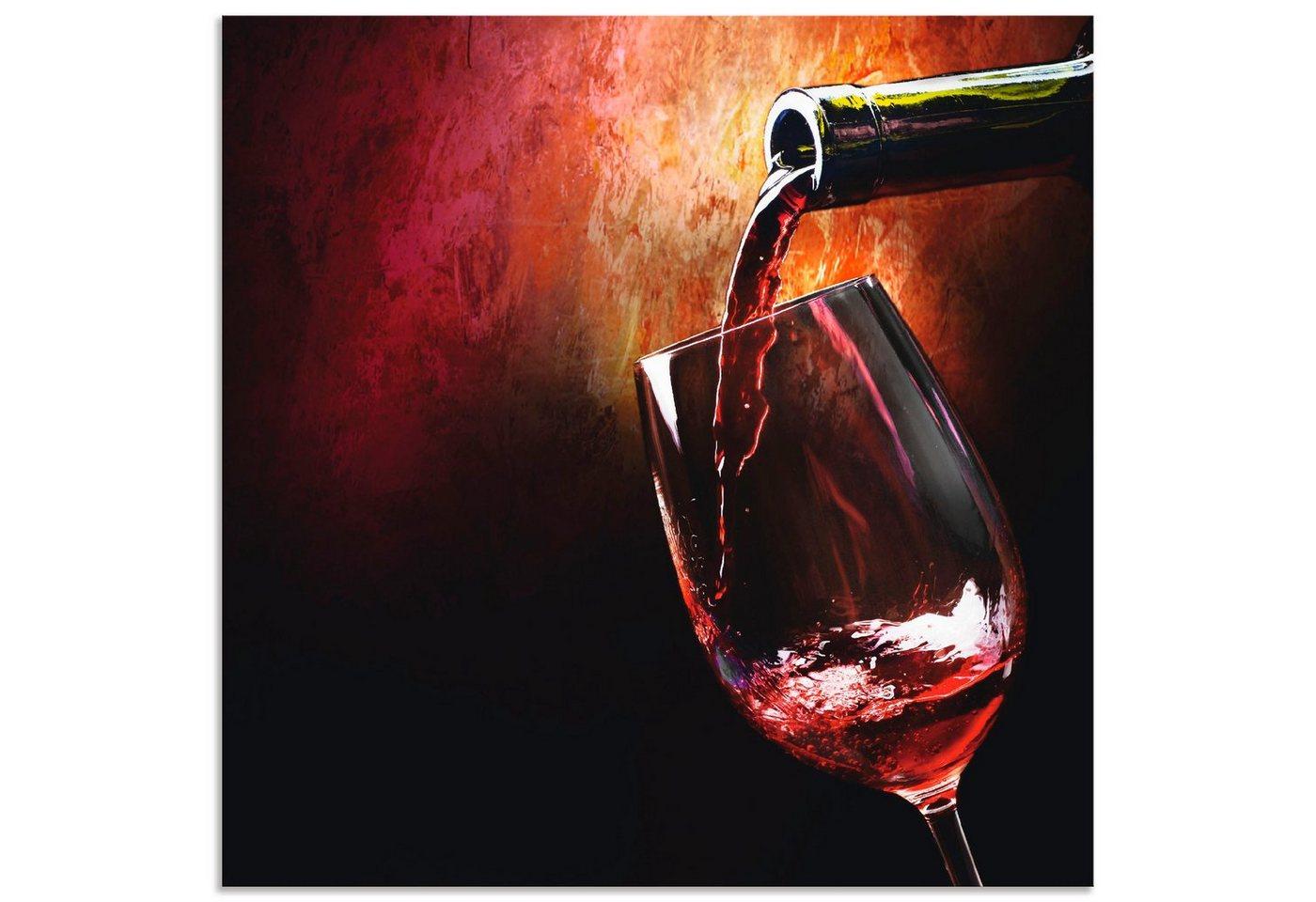
Artland Wandbild Wein - Rotwein, Getränke (1 St),...
25,99 €
OTTO
ab 2,95 Versandkosten
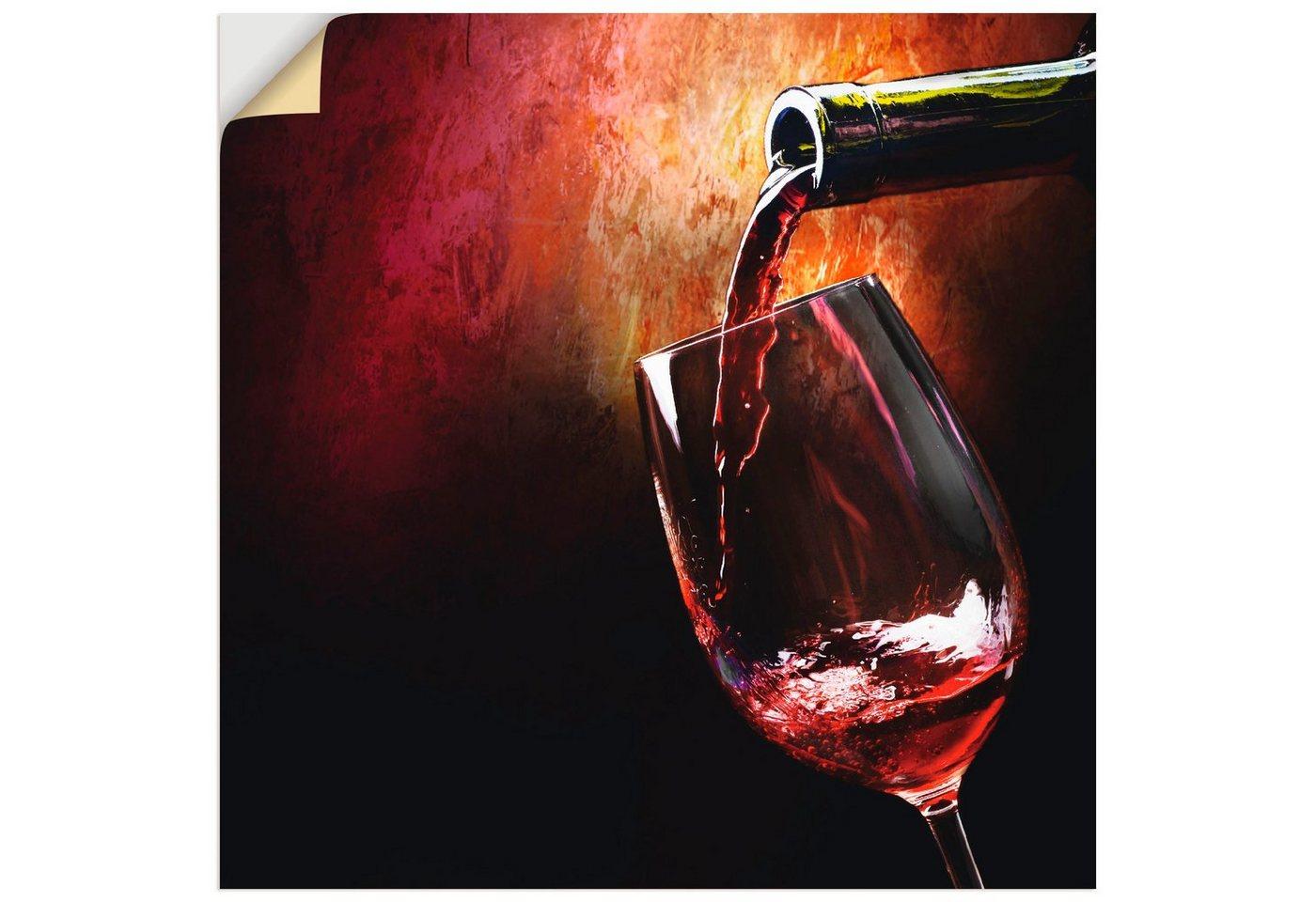
Artland Wandbild Wein - Rotwein, Getränke (1 St),...
24,99 €
OTTO
ab 2,95 Versandkosten

Artland Wandbild Wein - Rotwein, Getränke (1 St),...
32,99 €
OTTO
ab 2,95 Versandkosten
SIKORA Christbaumschmuck BS745 Rotwein Weinflasche...
36,95 €
OTTO
ab 4,95 Versandkosten